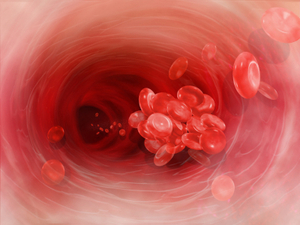
Deep venous thrombosis is the development of a blood clot in the large, deep veins of the lower leg and thigh. Thrombi can cause tissue injury due to vascular occlusion or distal embolization. However, venous obstruction can be offset by collateral blood vessels. Thrombi can also cause local pain and edema due to the blockage of blood flow. If the clot breaks off and travels through the blood, it is referred to as an embolism. An embolism can become trapped in the brain, lungs, or heart leading to major injury. Pulmonary embolus (PE) is a common complication and life threatening if not treated quickly with anticoagulants. PE presents with shortness of breath, chest pain, and cough with blood in sputum.
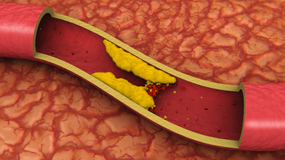 DVT can occur with stasis or in hypercoaguable states. It is commonly seen following trauma, surgery, or burns, which contribute to decreased physical activity, damage to vessels, and release of procoagulant substances from tissues. Reduced physical activity causes a decline in the milking action of lower leg muscles and slows venous return. Risk factors for DVT include advanced age, bed rest, immobilization, smoking, birth control pills, family history of blood clots, fractures in the pelvis or legs, giving birth within the last 6 months, heart failure, and obesity. To prevent DVT, patients should move their legs during long flights or when they are immobile for long periods of time.
DVT can occur with stasis or in hypercoaguable states. It is commonly seen following trauma, surgery, or burns, which contribute to decreased physical activity, damage to vessels, and release of procoagulant substances from tissues. Reduced physical activity causes a decline in the milking action of lower leg muscles and slows venous return. Risk factors for DVT include advanced age, bed rest, immobilization, smoking, birth control pills, family history of blood clots, fractures in the pelvis or legs, giving birth within the last 6 months, heart failure, and obesity. To prevent DVT, patients should move their legs during long flights or when they are immobile for long periods of time.
Although many DVTs are asymptomatic, they can recur. Some individuals suffer from post-phlebitic syndrome, which involves chronic pain and swelling in the leg. The major symptoms of DVT include changes in a patient’s leg such as redness, increased temperature, pain, and tenderness. Diagnosis is based on the physical exam, which should demonstrate a red, swollen leg. Diagnostic tests include a D-dimer blood test along with other blood tests to check for hypercoagulability such as activated protein C resistance, anti-thrombin III levels, antiphospholipid antibodies, and genetic testing for mutations with a predisposition towards blood clots. Imaging studies of the legs include Doppler ultrasound, plethysmography, and radiography.
The primary treatment for DVT is anti-coagulants, also known as blood thinners. They prevent the formation of new clots and the growth of old clots. However, they cannot dissolve existing clots. Patients are more likely to bleed on these medications. Heparin is an IV administered anticoagulant given in a hospital setting. Warfarin (Coumadin) is an oral anticoagulant that takes several days to work; thus, Heparin cannot be stopped until Warfarin is functioning at an effective dose for a minimum of two days. Many patients wear pressure stockings on their legs to improve blood flow and decrease their risk of DVT. When medications are ineffective, patients may need to undergo surgery. A filter can be placed in the body’s largest vein to prevent thrombi from migrating to the lungs. Also, surgery may be necessary to remove large thrombi.