Posted by Dr. Jack Sacks on May 24, 2018.
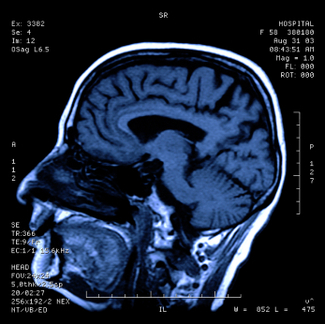
The prevalence of brain injury in the United States is alarming as it is the second leading cause of disability in the country. Often referred to as the silent epidemic, approximately 3.17- 5.3 million Americans suffer from traumatic brain injuries, another 4.7 million have brain injuries from strokes, and another 500,000 have cerebral palsy (brain injury due to an event of oxygen deprivation). Causes of brain injury that may give rise to a medical malpractice lawsuit are further described below:
 Brain Injury from Birth: a medical malpractice lawsuit may arise may when a child’s brain is negligently deprived of oxygen during pregnancy, labor and delivery. This may result in the child later developing cerebral palsy, mental retardation, seizures, blindness, deafness, and learning disabilities. Oxygen deprivation that injures a baby’s brain may arise from any of the following events:
Brain Injury from Birth: a medical malpractice lawsuit may arise may when a child’s brain is negligently deprived of oxygen during pregnancy, labor and delivery. This may result in the child later developing cerebral palsy, mental retardation, seizures, blindness, deafness, and learning disabilities. Oxygen deprivation that injures a baby’s brain may arise from any of the following events:
*Compression of the umbilical cord during delivery
*Maternal Infection present during the pregnancy or delivery
*Placental abruption or uterine rupture prior to birth
*Maternal high blood pressure during the pregnancy (preclampsia)
*Breeched vaginal position of the baby (feet first rather than head first)
*Improper administration or doasage of epidural or labor inducing drugs during the delivery
*Failure to timely perform an emergency c-section
*Fetal macrosomia (oversized baby) unable to navigate the birth canal
Brain Injury in Adults and Children: a medical malpractice lawsuit may arise as a result of errors in diagnosis and treatment of a serious medical condition. A few of the causes of brain injury in children and adults that may involve medical malpractice include:
*Medication errors
*Anesthesia errors
*Surgical errors
*Radiology errors
*Emergency room errors
*Delay in diagnosis/treatment of heart attack or cardiac arrest
*Delay in diagnosis/treatment of a stroke, aneurysm, or blood clot
*Delay in diagnosis/treatment of meningitis or encephalitis
*Delay in diagnosis/treatment of a spreading infection or abscess
*Delay in diagnosis/treatment of internal bleeding
*Delay in diagnosis/treatment of hydrocephalus
*Delay in diagnosis/treatment of diabetes/diabetic coma/insulin shock
In addition to the above mentioned causes of brain injury, many other errors involving patient treatment and care may give rise to a lawsuit. One of the most common causes occurs when a hospital patient or nursing home patient falls (due to inadequate protective measures) and the patient suffers a traumatic brain injury. In fact, falls are the leading cause of traumatic brain injury in our country surpassing even motor vehicle accidents. For a detailed guide to the incidence, prevalence, and epidemiology of brain injury, seeEssential Brain Injury Guide prepared under the auspices of the Brain Injury Association of America.